GS2 – Social Sector – Health – Diseases
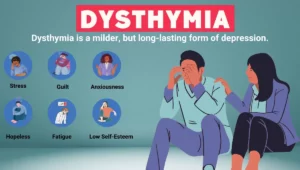
Dysthymia, a prolonged variant of depression, often goes unrecognized or is misunderstood due to its subtle yet chronic nature.
Definition and Nature
Dysthymia, medically termed Persistent Depressive Disorder (PDD), refers to a long-lasting, milder form of depression. In adults, symptoms persist for at least two years, while in children and adolescents, they last one year or more.
Key Characteristics
- Unlike occasional sadness, dysthymia manifests as a chronic mood disturbance impacting sleep, appetite, self-worth, decision-making, and overall emotional well-being.
- Often misjudged as a ‘low-grade’ issue, its intensity is lower than major depressive disorder but it is more persistent, making it equally impairing.
Concept of Double Depression
When a person with dysthymia experiences a major depressive episode on top of their ongoing symptoms, it is referred to as double depression, complicating diagnosis and treatment.
Differentiation from Major Depression
- Dysthymia generally does not involve anhedonia (inability to experience pleasure) or significant motor function alterations, which are often present in major depression.
- Major depression is diagnosed when a person displays five or more symptoms over a minimum of two weeks.
Vulnerable Populations
- Women are nearly twice as likely to develop dysthymia as men.
- Individuals with coexisting mood disorders, anxiety, substance dependence (like alcoholism), or bipolar disorder are also at increased risk.
Symptoms of Dysthymia
Typical signs include:
- Chronic low energy,
- Disturbed sleep patterns,
- Altered appetite (either overeating or loss of appetite),
- Persistent low self-esteem,
- Poor focus, and
- A deep sense of hopelessness.
Treatment Strategies
A comprehensive approach combining pharmacological and psychological interventions is essential for effective treatment.
- Medications: Often includes Selective Serotonin Reuptake Inhibitors (SSRIs) and dual-action antidepressants that target neurotransmitter imbalances.
- Psychotherapy: Techniques such as Cognitive Behavioral Therapy (CBT), interpersonal therapy, psychodynamic approaches, and supportive counseling help patients manage and cope with long-term symptoms.
Underlying Causes
- The disorder arises from a complex interplay of factors, including chemical imbalances in the brain, genetic tendencies, emotional trauma, prolonged stress, and social isolation.
- While it is seen to run in families, specific genetic markers have not been definitively identified.